Psychedelics, meditation & wellbeing retreat
“The will to win is not nearly as important as the will to prepare to win.
” - Anonymous
Description ...

“The will to win is not nearly as important as the will to prepare to win.
” - Anonymous
Description ...
"Those friends thou hast, and their adoption tried, grapple them unto thy soul with hoops of steel."
"This above all: to thine own self be true, and it must follow, as the night the day, thou canst not then be false to any man." Both quotations by Polonius in Shakespeare's "Hamlet"
"You've got to spread joy up to the maximum. Bring gloom down to the minimum. Otherwise pandemonium ... Liable to walk upon the scene". Bing Crosby sings
"You've got to accentuate the positive. Eliminate the negative. Latch onto the affirmative. Don't mess with Mr In-Between". Bing Crosby sings!
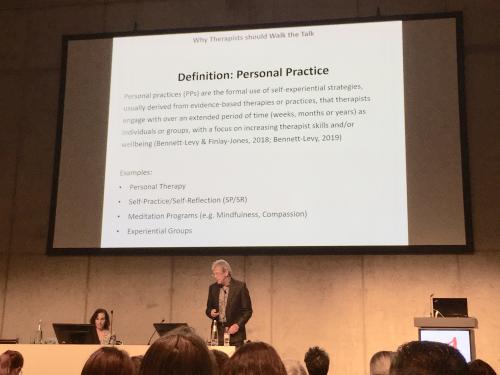
Well this was a fascinating day ... I went to my friend James Bennett-Levy's fine symposium on "Self-practice/self-reflection (SP-SR) at 18: an experiential training strategy maturing into adulthood", then on to an interesting & helpful symposium discussing broader applications of Arnoud Arntz's imagery approaches - "Efficacy of imagery rescripting as a transdiagnostic intervention". And to complete the morning's cornucopia I was back listening to James delivering a barn-storming plenary on "Personal practice: why therapists should walk the talk." I sat with Judy, James's wife, and we considered standing to applaud at the end but decided this might be a bit over-the-top, even if richly deserved.
I read a lot of research. When I find an article of particular interest I download it to my bibliographic database - Endnote - which currently contains well over 27,000 abstracts. I also regularly tweet about emerging research, so following me on Twitter, Facebook or Google+ (click on the relevant icon at the top of this web page) will keep you up to speed with some of what I'm finding interesting. Additionally you can view this highlighted research by visiting Scoop.it (click on the "it!" icon at the top of the page). At Scoop.it, I stream publications into five overlapping topic areas: Cognitive & General Psychotherapy, Depression, Compassion & Mindfulness, Healthy Living & Healthy Aging, and Positive Psychology ...
I read a lot of research. When I find an article of particular interest I download it to my bibliographic database - Endnote - which currently contains well over 26,500 abstracts. I also regularly tweet about emerging research, so following me on Twitter, Facebook or Google+ (click on the relevant icon at the top of this web page) will keep you up to speed with some of what I'm finding interesting. Additionally you can view this highlighted research by visiting Scoop.it (click on the "it!" icon at the top of the page). At Scoop.it, I stream publications into five overlapping topic areas: Cognitive & General Psychotherapy, Depression, Compassion & Mindfulness, Healthy Living & Healthy Aging, and Positive Psychology.
I read a lot of research. When I find an article of particular interest I download it to my bibliographic database - Endnote - which currently contains well over 26,000 abstracts. I also regularly tweet about emerging research, so following me on Twitter, Facebook or Google+ (click on the relevant icon at the top of this web page) will keep you up to speed with some of what I'm finding interesting. Additionally you can view this highlighted research by visiting Scoop.it (click on the "it!" icon at the top of the page). At Scoop.it, I stream publications into five overlapping topic areas: Cognitive & General Psychotherapy, Depression, Compassion & Mindfulness, Healthy Living & Healthy Aging, and Positive Psychology.
At our eighth & last session of the Compassion, wisdom & wellbeing training, we reviewed the journey we've been on together over the last couple of months. We looked at what each of us personally had found most interesting & valuable. The weekly reflection sheets that we'd filled in could make it easier to remember the variety of areas we've explored.
These home practice suggestions link with the seventh session of the Compassion, wisdom & wellbeing training. There are seven home practice requests for the fortnight until our 8th & last evening together.