The potential value of rescripting images in chronic pain & other distressed states like depression & anxiety: treatment
Last updated on 16th April 2013
I have recently written a couple of blog posts - "The potential value of rescripting images in chronic pain & other distressed states like depression & anxiety: introduction" and "The potential value of rescripting images in chronic pain & other distressed states like depression & anxiety: assessment". The posts were triggered by Clare Philips' research paper "Imagery and pain: The prevalence, characteristics, and potency of imagery associated with pain". In today's post I would like consider potential treatment implications of this work - for pain sufferers, but also for distressed states more generally . A good place to start is by introducing Clare Philips' linked second paper (written with co-author Debbie Samson) "The rescripting of pain images".
The paper's abstract reads "Background: The majority of pain sufferers experience images when in pain. The most distressing of these images (the Index image) provokes intense emotional reactions, appraisal shifts, and increases in pain. The ability of pain sufferers to rescript their Index images, and the consequences of doing so, remain to be determined. Aims: To assess the effects upon emotions, appraisals and pain experience of rescripting Index images in pain sufferers. Method: The Index images of a group of 55 pain sufferers were assessed using a voluntary image induction procedure (VIE) to obtain basal levels of pain, appraisal and emotion. Participants were than randomly allocated to one of two groups: Rescripted Image repetition or Index Image repetition. The two groups were compared on their responses to their Index and Rescripted images respectively. Results: The participants found it easy to rescript their distressing Index images. During rescripting, they reported dramatic reductions in emotion, negative appraisals, and pain. The clinically and statistically significant decrements in pain were found independent of reductions in emotion. The pain levels during rescripting were significantly below their basal levels, with 49% reporting no pain at all while viewing a rescripted image. These changes were not a function of image repetition. Conclusion: Index images of pain sufferers can be easily elicited and rescripted. Rescripting leads to remarkable reductions in emotion, cognitions and pain levels that are not attributable to image repetition. The significant reductions in pain were independent of reductions in emotion. The implications of these results for CBT approaches to pain management are considered."
Wow ... this is a potentially exciting set of findings. What was involved in the imagery rescripting here and how might this be relevant both for other chronic pain sufferers and also potentially for people struggling with other distressing problems like depression & anxiety? I notice a bit of circularity & cross-fertilisation in these questions. So I'm interested in how this research on pain might inform broader imagery rescripting interventions for other disorders too. However Philips & Samson's pain research is itself triggered by extensive work already done on anxiety & depression. So the authors write "In the last decade, there has been a rapid expansion of research and clinical work on image cognitions. Over 30 years ago, Beck described "....maladaptive ideation.....in pictorial form" ... but the full significance of the potency and role of imagery has only recently been recognized. The experimental studies of Holmes and Mathews (2010) confirm that images are more potent - negatively and positively - than thoughts of comparable content. In clinical groups, images are found to be intrusive, spontaneously occurring cognitive events with remarkable clarity, similarity and unchanging content ... Their emotional potency does not appear to habituate. Studies of how these distressing images can be modified by a cognitive procedure called Rescripting are now appearing ... Rescripting procedure requests patients to change their distressing index images into a preferred benign form. The patient is asked to describe their recurrent most distressing image in detail and is then encouraged to change the image and transform it to a preferred benign version. There are two distinguishable aspects of the rescripting procedure: sensory re-description and cognitive re-appraisal ... The Index image (the most distressing /powerful image) loses some or all of its emotional potency by this relatively simple and straight forward cognitive method."
Mm ... I don't see "imagery rescripting" quite like this. I guess I see a more complex picture ... the recent post I wrote "Imagery, associative networks, embodied cognition and the transformation of meaning" illustrates this pretty well. However I like the way Philips & Samson respected the sufferers and, in this research, asked them how they would like to change their images. When we look more broadly at potentially important images linked to a variety of types of psychological as well as physical pain, often the distress associated with the image can be very strong. Posttraumatic stress disorder is the classic example here. In quite an extended post I wrote last autumn - "Working with traumatic memories: trauma-focused CBT and an introduction to rescripting" - after a workshop with PTSD expert Nick Grey, I said "At present I would go with incorporating new information & imagery rescripting (sometimes guided by exploration of possible posttraumatic growth) as worthwhile interventions to be able to add to straightforward exposure style imaginal reliving. However I would also try to be a little cautious & humble about rushing in too quickly with rescripting. Working at the great emotional depth that is often the challenge and the profound privilege of trying to help people suffering from PTSD reminds me of something a sculptor friend once said to me. I was asking him about how he worked with a block of stone to carve out the eventual shape he had in mind. He said that yes he would chisel in knowing what figure he hoped would emerge, but he also tried to be sensitive & responsive to what evolved as he worked with the stone. This is my experience in strongly emotional phases of therapy. I try to be soft, sensitive, aware as the "emotional spray is whipping into my face". At times the most creative, helpful changes emerge spontaneously from the client, with new healing insights & directions coming out of the reliving/revisiting journey (no doubt helped by the discussions we have had about how & what we're trying to achieve therapeutically before we dived into the emotional rapids). Rightly or wrongly, I suspect that some cognitive-behavioural therapists are a bit awkward in situations of high emotion and may slap on pre-programmed additional information & rescripting too quickly & formulaically. There's an interesting research question here that will probably never be explored. See the posts " ... cathartic work from the inside" and " ... cathartic work from the outside" for more on this. For practical suggestions about how best to go about working with imagery in PTSD treatment there are many good resources. Examples include "A casebook of cognitive therapy for traumatic stress reactions" (edited by Nick) and the "Oxford guide to imagery in cognitive therapy" ... See too the posts on trauma-focused CBT's use of writing and site visits/discrimination training."
OK, I've made quite a leap here from the apparently often quite emotionally cool rescripting that Philips & Samson describe in this paper on helping chronic pain sufferers to the potentially hugely charged interactions often experienced when working with PTSD sufferers who may have been abused, raped, watched loved ones die, or been in other emotional furnaces. So with patients in this pain research study "To obtain their
Rescripted version they were asked "How would you rather see the image?" or "How would you prefer it to have been?" and encouraged to describe in full what this image would entail. All details were recorded." And the authors comment "simple rescripting was easily accomplished".
In the section of their paper entitled "Limitations and implications for further research", they write "A limitation of this study was the exclusive focus on sensory rescripting without assessing the meaning which the participants attached to their Index images. Now that significant and sizeable changes have been found with sensory rescripting alone, research on the re-appraisal of Index images and the effect of rescipting on image appraisal will be of interest. It is likely that combining cognitive re-appraisal with sensory rescripting will lead to even stronger results." Well, maybe ... I would be still be extremely happy if the short-term results of imagery rescripting that they report here didn't get much stronger ... if only they are found to be replicable for other pain sufferers, and for people struggling with other kinds of disorder (e.g. depression & anxiety), and that the short-term benefits translate into longer-term gains.
The short-term gains that they found with this simple rescripting procedure were extraordinary. They wrote "When the participants first formed their Index image, they experienced negative emotions and increased pain. However after rescripting their images, they experienced substantial reductions in the negative emotions, pain and appraisals. Remarkably 49% (of the 55 participants) reported no pain at all during the rescript. In the control group (G-I), repetition of the Index image was not accompanied by any of these reductions. All participants found the rescripting procedure easy to carry out, and pleasurable. The large majority had little hesitation in elaborating how they would prefer to see their Index images. A few needed some encouragement/suggestions, but no discussions of image meanings were undertaken. Only sensory details were suggested. A few participants resorted to magical realism ideas when they were unable to decide on a preferred sensory alternative. The effects of the rescripting upon the measures of emotion, appraisal and pain experience were statistically significant and clinically substantial. The changes produced did not merely replicate the reduction in emotions reported in studies of other disorders using rescripting (Hackmann et.al., 2004, Brewin et.al., 2005, Clark and Wells,1995, Ehlers et.al.,2000) but also revealed a significant change in pain levels. The latter were shown to be independent of the significant reductions of anxiety and sadness. Thus a pain experience was demonstrated to be reduced by a relatively simple manipulation of a cognitive variable: image content. The pain decrements were fast, easily produced and dramatically large."
So averaging the changes seen in the two assessed groups, shifts from baseline to imagining the original pain-associated image, to imagining the rescripted image were for anxiety level, from 28.4 to 63.65 to 7.25; for sadness, from 32.75 to 64.15 to 3.6; for anger, from 32.3 to 49.2 to 3.7; and for pain from 45.7 to 56.05 to 13.25. Stunning.
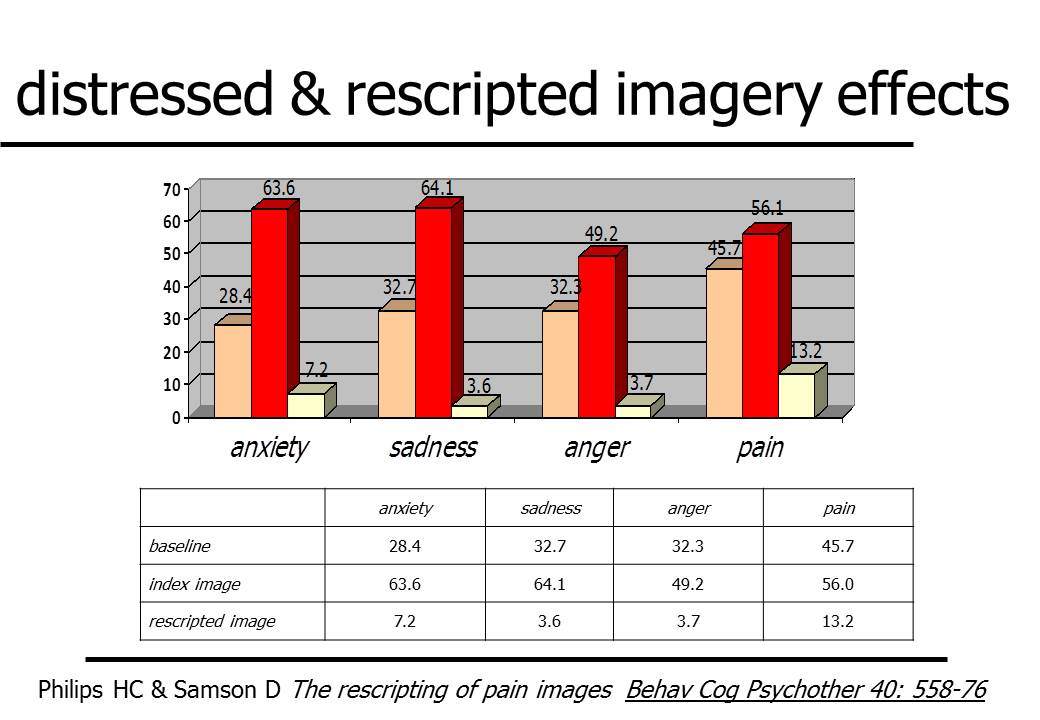
(this chart is downloadable as a PDF file & as a Powerpoint slide)
And the authors say "Encouraging post-session practice of the rescripted benign alternative is likely to consolidate treatment progress, and reduce the frequency of distressing images. As the experiment was undertaken in one session, participants made only one attempt at developing their preferred image. In a treatment context, and with cognitive reappraisal, it seems likely that participants would progressively refine their preferred image. A hint of this process occurred in this study. Having completed a rescripted image description and evaluated its effects on the analogue scales, one participant wanted to make an addition to his image. This illustrates that relatively small changes can have large effects on image potencies. Index Image: "I see myself all alone ..at home ..unable to do anything. I am just watching the television." Initial rescript: "I see myself returning to my job. I'm not limping. I look strong and well...I am smiling and happy." Addition... "all my co-workers and pals are coming round me. My friend puts his arm around me to welcome me back." Remarkable reductions in anxiety and sadness resulted from this addition. Meanings of the Index images were not being assessed, but from this potent addition one would predict that social isolation and exclusion consequent upon his injury were important aspects of his Index image. This had not been evident in the Index image description, in which co-workers where absent from the image."
Fascinating. This research links through to so many other potentially helpful areas. For example, work on posttraumatic growth might very usefully inform imagery rescripting - see "Writing (& speaking) for resilience & wellbeing: personal growth". Research on embodied cognition can be highly relevant too, as can be the development of a personalized brief imagery/meditation practice. This work by Clare Philips & Debbie Samson adds to the growing series of studies demonstrating the particular value of working with imagery in relieving a wide variety of distressed states. It cries out to be replicated and extended.
(Downloadable resources include an imagery assessment questionnaire available both as a PDF file and as a Word doc, a table to track changes during rescripting available as a PDF file and as a Word doc, a frequency/severity assessment scale also available both as a PDF file and as a Word doc, the text of the first & second of this blog sequence as a PDF file and as a Word doc, and the text of the third blog on treatment as a PDF file and as a Word doc)
